The gut-brain axis
“Let
food be thy medicine and medicine be thy food.”
― Hippocrates 2400 BC
(Before Christ) or 2400 BCE (Before Common Era)
Hippocrates – the father of medicine – how erudite! The same Hippocrates who said that epilepsy can be cured by fasting and this method proved to be the precursor of the modern ketogenic diet.
We also know that the gastro-intestinal system has a major effect on our mood, behavior, cognition and higher intellectual functions .
“I have a gut feeling”, “I feel butterflies in my stomach” are ancient sayings but in the last few decades a lot of insight has developed in the relationship of the gut and the brain called the gut-brain axis or GBA.
Is the stomach a second brain?

In the first part of this series we will explore the fascinating world of this axis long known to Ayurved
Scientifically what is the physiology of the gut brain axis and how do they communicate with each other.
You have 2 brains
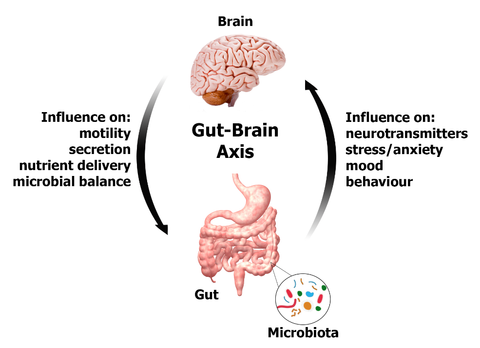
The GBA controls and coordinates the gut activity. It also links emotion and cognition with enteric functions and mechanisms like immune mechanisms, intestinal permeability and enteric reflexes and entero-endocrine functions. The gut and the brain communicate through nerves, chemicals (hormones and neurotransmitters) and immune system. The brain has around 100 billion neurons each of these have around 10,000 synapses or communicating points. So, there are around 1 quadrillion communicating points. The gut on the other hand has around 500 million neurons. This complex system comprises of the CNS (brain and spinal cord) autonomic nervous system (ANS) enteric nervous system (ENS) and the hypothalamic pituitary axis (HPA).
They communicate through the ANS namely sympathetic and parasympathetic nerves. The afferents from the lumen and intestinal wall pass primarily through the vagus nerve, but also the enteric and spinal nerves. The brain in turns communicates to the gut (efferent) through the same ANS.
The role of vagus nerve in disease – some observations and research:
- Persons with Chron’s disease and Irritable Bowel syndrome have lower vagal tone.
- Examination diarrhea is a common phenomenon and stress is known to inhibit vagal nerve signals.
- Probiotic action on stress is reduced if the vagal nerve is severed.
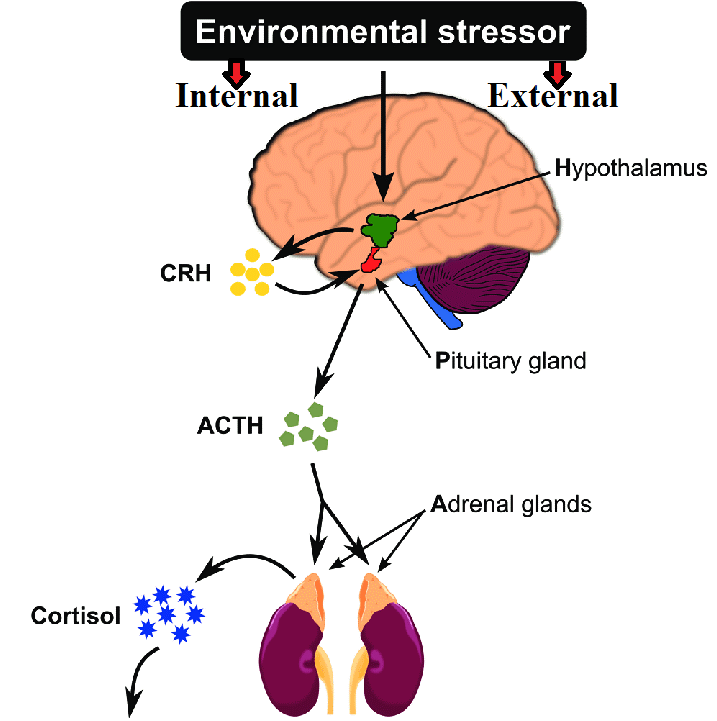
The HPA on the other hand is the hormonal arm of this axis. It is activated by stress (both internal and external or environmental) and pro-inflammatory cytokines. Through this CRF is secreted which in turn causes ACTH release. This stimulates the adrenals leading to cortisol release.
Norepinephrine (NE), epinephrine (E), dopamine (DA), and serotonin have recently been a topic of interest because of their roles in the gut physiology and their potential roles in gastrointestinal and central nervous system pathophysiology. Mittal et al.
Role of these neurotransmitters:-
Able to regulate and control :-
- Blood flow
- Gut motility
- Nutrient absorption
- Gastrointestinal innate immune system
- The microbiome.
Neurotransmitters are produced in the gut. For example, 90% of the serotonin (the chemical that gives the ‘feel good’ phenomenon) is produced in the gut. . Serotonin is secreted by the entero-chromaffin cells in the gut. It is seen that a serotonin dysfunction if the gut can influence mood, sleep, behaviour and cognition.
Thus both nervous and hormonal mechanisms play a role in the brain control of enteric enzyme release, enteric neurons, epithelial cells, smooth muscle cells, intestinal permeability, cells of Cajal and entero-chromaffin cells. In the next section we will explore how the gut influences epilepsy.
References:-
Mittal et al. Neurotransmitters: The critical modulators regulating gut-brain axis J Cell Physiol. 2017 September ; 232(9): 2359–2372
