Now that we have looked at the gut brain axis anatomy and physiology let us turn to the relationship to epilepsy. Anecdotal evidence has been around and several patients’ complain that constipation is a seizure trigger. However there is some research proof to this observation.
Constipation induced by loperamide and clinidum caused a decrease in threshold to clonic seizure in the intravenous pentylenetetrazole seizure model. Moreover loperamide- or clidinium-induced constipation decreased latencies to, clonic, and tonic seizures and death in the intraperitoneal pentylenetetrazole model of mice. Serum ammonia levels were slightly elevated in both loperamide- and clidinium-treated mice. In conclusion, both made mice more prone to seizure which might confirm the belief of patients and physicians about constipation as a trigger of seizure. (Epilepsy and behavior – Constipation enhances the propensity to seizure in pentylenetetrazole-induced seizure models of mice. Leila Moezi, Fatema Pirsalami and Soroor Inaloo)
The human evidence of gut microbiota brain relationship is still not very clear.
The interest sprung from a 22 year old with Crohn’s disease and 17 years of uncontrolled seizures. A fecal microbiota transplant (FMT) was undertaken for the Crohn’s. There was a 20 month seizure free period following this even though anti-seizure medication was withdrawn prior to FMT.
This fuelled interest in the role of intestinal dysbiosis in epilepsy.
Intestinal microbiota has a large role in health. They play a large role in immune systems and also in fighting pathogens. Their genes are 150 times more than the human genome and thus many enzymatic reactions are caused by these bugs. In addition, they increase healthy vitamins and short chain fatty acids (SFA) like butyrate. This has direct positive effect on immune mechanisms, maintenance of the epithelial barrier (anti-‘leaky gut’) and enhanced satiety after a meal. They are also protective in various conditions like colorectal cancer, irritable bowel syndrome, diabetes and obesity. Thus, stimulating butyrate production enhances health in humans.
This microbiota-gut-brain axes is being studied extensively to understand and use this for improving the human intestinal microbiota. This complex communication is through the autonomic and enteric nervous system.
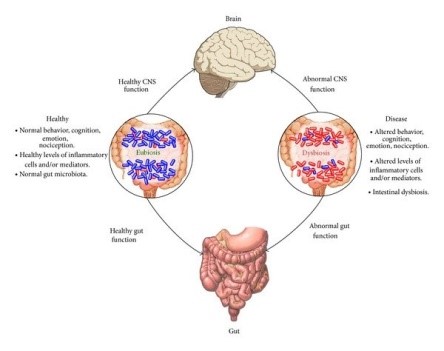
Microbiota flora is heavily dependent on the environment in the gut and this can be tweaked to our advantage. The microbiota have a large role in emotional make-up, cognitive skills and mood of the individual and can contribute to the spectrum of anxiety and depression. The gut microbiome in persons with epilepsy differs in those with drug –sensitive epilepsy and in those with drug-resistant epilepsy. For example, firmicutes are more in those with drug-resistant epilepsy. Bifidobacteria and lactobacillus is more in those with less than four seizures per year in both groups.
In the next part we will look at the role of the ketogenic diet and its effect on microbiota. Whether some of the anti-seizure effect of KD is through this effect will be explored further. Dr. J. Nathan is working with the Manipal Research Centre on this exciting aspect of KD.
